Introduction

Coverage and Use of Medicare and Telehealth During the COVID-19 Pandemic, as well as Future Options: During the COVID-19 pandemic, telehealth, or the delivery of health care services to patients by physicians who are not in the same place, has seen a significant increase in utilization among both privately insured patients and Medicare beneficiaries. Prior to the pandemic, conventional Medicare only covered telehealth services for patients residing in rural regions, with limits on where these services could be received and which providers could be compensated to offer them.
In early 2020, shortly after the federal government declared a public health emergency due to COVID-19, Congress and the Centers for Medicare & Medicaid Services (CMS) expanded traditional Medicare’s coverage of telehealth services to make it easier for beneficiaries to get medical care and reduce their exposure to coronavirus in health care settings. Unless officials take steps to continue the extended coverage when the public health emergency ends, Medicare’s coverage of telehealth services will revert to the more limited availability that existed before the epidemic.
This brief gives a review of the modifications made to Medicare’s telehealth coverage during the COVID-19 pandemic in light of the fast, but time-limited, extension of telehealth coverage under regular Medicare. It also includes a fresh analysis of Medicare members’ use of telehealth during the summer and autumn of 2020, as well as difficulties and questions about expanding telehealth coverage beyond the public health emergency under conventional Medicare. Our research of beneficiaries’ usage of telehealth services is based on data from the CMS Medicare Current Beneficiary Survey (MCBS) Fall 2020 COVID-19 Supplement, which included data from Medicare beneficiaries residing in the community. Unless otherwise stated, all differences indicated in the text are statistically significant. (For further information, see Data and Methods.)
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
Key Findings
- Nearly two-thirds (64 percent or 33.6 million) of Medicare beneficiaries with a regular source of care (95 percent), such as a doctor or other health professional, or a clinic, say their provider now offers telehealth appointments, up from 18 percent who said their provider offered telehealth before the pandemic. However, nearly a quarter of Medicare beneficiaries (23%) say they have no idea whether their provider provides telemedicine sessions, and this figure is higher among those who reside in rural regions (30 percent ).
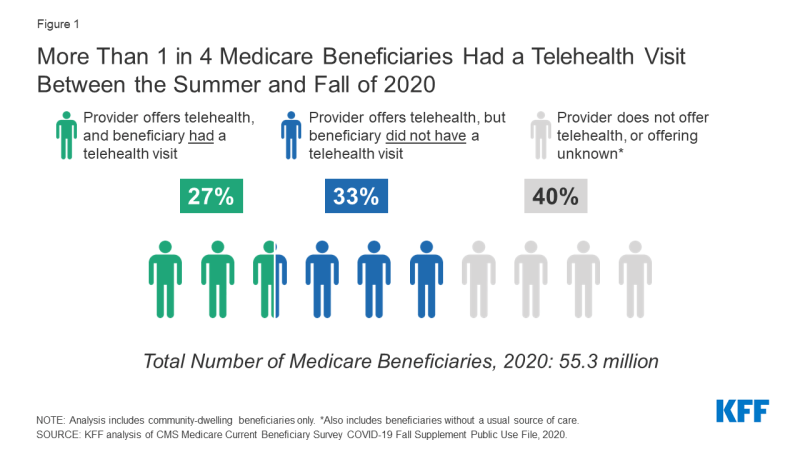
- Nearly half (45 percent) of the 33.6 million Medicare beneficiaries with a regular source of care who stated their provider presently provides telehealth appointments claimed they had a telemedicine visit with a doctor or other health professional during the summer (July) and fall (Fall) of 2020. This amounts to slightly over a quarter of all community-dwelling Medicare and Medicare Advantage beneficiaries (27 percent or 15 million) using telemedicine throughout this time period (Figure 1).
Figure 1: Between the summer and fall of 2020, more than 1 in 4 Medicare beneficiaries had a telehealth visit.
- Medicare beneficiaries under the age of 65 who qualify for Medicare due to a long-term disability (53 percent), beneficiaries enrolled in both Medicare and Medicaid (55 percent), Black (52 percent) and Hispanic (52 percent) beneficiaries, and those with six or more chronic conditions were more likely to report using telehealth (56 percent ). Greater rates of telehealth usage may be linked to higher total health care use for particular groups, such as Medicare-Medicaid participants and those with numerous chronic diseases. There was no difference in reported telehealth utilization between conventional Medicare and Medicare Advantage enrollees (44 percent and 45 percent, respectively).
- A majority (56%) of Medicare beneficiaries who had a telehealth visit say they received care just over the phone, while a lower percentage (28%) say they received care through video or both video and telephone (16 percent ). Medicare beneficiaries aged 75 and older (65 percent), Hispanic beneficiaries (61 percent), those residing in rural regions (65 percent), and those enrolled in both Medicare and Medicaid (65 percent) were more likely to have a telehealth visit utilizing only the telephone (67 percent ).
Background on Medicare Coverage of Telehealth and Changes under the COVID-19 Public Health Emergency
Prior to the COVID-19 epidemic, typical Medicare reimbursement of telehealth services was restricted. There were constraints on how these services could be offered and which beneficiaries could access them, thus Medicare-funded for about 100 telehealth programs. Outside of a public health emergency, such restrictions do not apply to Medicare Advantage plans, which have the freedom to provide extra telehealth benefits not covered by regular Medicare (see below for more information).
Prior to the pandemic, conventional Medicare users’ use of telehealth services was extremely low, with only 0.3 percent of Part B beneficiaries using telehealth services in 2016, accounting for only 0.4 percent of traditional Medicare Part B spending. Similarly, prior to the pandemic in February 2020, a review of typical Medicare primary care visits indicated that just 0.1 percent of these visits were delivered via telehealth.
Before the public health emergency, telehealth services were generally available only to beneficiaries in rural areas originating from a health care setting, such as a clinic or doctor’s office. Beneficiaries in urban areas were ineligible for telehealth services, and beneficiaries could not receive telehealth services in their own homes. During a public health emergency, beneficiaries in any geographic area can receive telehealth services, and can receive these services in their own home, rather than needing to travel to a “distant site” (i.e., a health care setting).
Which traditional Medicare beneficiaries can receive telehealth services and where?
Prior to the public health emergency, telehealth services were mainly only offered to rural beneficiaries who came from a health care facility like a clinic or doctor’s office. Telehealth services were not available to beneficiaries in metropolitan areas, and beneficiaries could not get telehealth services in their own homes. During a public health emergency, beneficiaries in any geographic area can receive telehealth services, and can receive these services in their own home, rather than needing to travel to a “distant site” (i.e., a health care setting).
What technologies can traditional Medicare beneficiaries use to access telehealth services?
A telehealth visit must be done using two-way audio/video communications under Medicare’s current telehealth coverage, and the use of cellphones or audio-only telephones in lieu of video is not approved. Telehealth services may be provided without the use of extra equipment during the COVID-19 public health emergency by employing an interactive audio-video system, as well as cellphones with real-time audio/video interactive capabilities. Patients can also receive a limited number of telehealth services via an audio-only phone or a smartphone without video.
What type of providers can get reimbursed by Medicare for telehealth visits?
Only physicians and certain other practitioners (such as physician assistants, clinical social workers, and clinical psychologists) were eligible for Medicare payment for telehealth services provided to eligible beneficiaries in traditional Medicare prior to the public health emergency, and they had to have treated the beneficiary receiving the services within the previous three years. Any health care practitioner who is eligible to charge Medicare for professional services can perform and bill for telehealth services during a public health emergency, and they do not need to have previously treated the beneficiary.
During the COVID-19 public health emergency, federally recognized health centers and rural health clinics are also allowed to provide telehealth services to Medicare beneficiaries; previous to the pandemic, these settings were not authorized to provide telehealth services to Medicare beneficiaries.
What services can traditional Medicare beneficiaries receive through telehealth?
Traditional Medicare-covered around 100 services that could be delivered through telehealth before the public health emergency, including office visits, psychotherapy, and preventive health screenings, among other services. During the public health crisis, the list of eligible telehealth services covered by regular Medicare was enlarged to include emergency room visits, physical and occupational therapy, and other services. Patients can get some evaluation and treatment, mental health, and patient education services through audio-only telephone.
Are there additional services, other than telehealth, that are delivered virtually and covered by traditional Medicare?
Traditional Medicare supports brief, “virtual check-ins” (sometimes termed “brief communication technology-based services”) by telephone or recorded video image, as well as E-visits, for all beneficiaries, regardless of whether they reside in a remote region. Both of these services are more limited in scope than a complete telehealth visit and were not altered during the public health emergency. Virtual check-ins, for example, can only be reported by providers who have a prior relationship with the patient, they can’t be related to a recent medical visit (within the last 7 days), they can’t lead to a medical visit within the next 24 hours (or the next available appointment), and payment is only intended to cover 5-10 minutes of medical discussion..
How does Medicare pay providers for telehealth services?
Prior to the public health emergency, Medicare paid the same amount for telehealth services delivered in a non-facility setting, such as a clinician’s office, or in a facility setting, such as a hospital outpatient department, and the payment rate was based on the lower amount paid to facility-based providers for a service delivered in person.
(Because Medicare makes a separate payment to facilities to cover practice expenses such as physical space, medical supplies, medical equipment, and clinical staff time, the payment to facility-based providers for in-person services is lower than the payment to non-facility providers under Medicare’s physician fee schedule.) The reasoning behind selecting the lower facility payment figure for telehealth services was that practice expenditures for telehealth services should be lower than those for an in-person visit.
During a public health emergency, Medicare pays for telehealth services, including those delivered via audio-only telephone, as if they were administered in person, with the payment rate varying depending on the provider’s location, which means Medicare pays more for a telehealth service provided by a doctor in a non-facility setting than a doctor in a hospital outpatient department. This also implies that doctors in non-facility settings are being paid more for telehealth services during the public health emergency than they were before the public health emergency.
What do traditional Medicare beneficiaries pay for telehealth services?
During the public health emergency, beneficiary cost-share for telehealth services remained unchanged. Telehealth services are covered by Part B of Medicare, thus conventional Medicare beneficiaries who utilize them will be subject to the Part B deductible of $203 in 2021 and a 20% coinsurance. During the COVID-19 public health emergency, however, the HHS Office of Inspector General gave providers the option to lower or waive cost-sharing for telehealth sessions, albeit there is no publicly available data to show how many providers did so. Most typical Medicare recipients have supplementary insurance, which may cover part or all of the cost-sharing for eligible telehealth services.
How is telehealth covered under Medicare for beneficiaries and providers participating in alternative payment modes?
Separate from the time-limited expanded availability of telehealth services, CMS has given providers in some alternative payment models, such as Next Generation accountable care organizations (ACOs) and Medicare Shared Savings Program ACOs, more flexibility to provide care through telehealth, including billing for telehealth services provided to both urban and rural beneficiaries, as well as beneficiaries at home. Benefit enhancement waivers administered by CMS are used to offer telehealth flexibility in the Next Generation ACO experiment. Few Next Generation ACOs got and implemented telehealth exemptions between 2016 and 2018. (4 ACOs; 8 percent of all ACOs in the model).
How does coverage of telehealth services differ in Medicare Advantage?
Outside of the public health emergency, Medicare Advantage plans have been allowed to provide additional telehealth benefits not covered by regular Medicare, such as telehealth visits delivered to members in their own homes and services supplied outside of rural regions. By 2021, nearly every Medicare Advantage plan (98%) will have a telehealth benefit.
Medicare Advantage plans are paid a capitated sum to offer basic Medicare services covered under Parts A and B; legislative amendments enacted in 2020 allow plans to incorporate extra telehealth benefits in their bids for basic benefits beyond what conventional Medicare provides. As a result, the cost of extra telehealth services provided by Medicare Advantage plans is included in the capitated payment received by such plans.
In situations of catastrophe or emergency, such as the COVID-19 epidemic, Medicare Advantage plans have the authority to waive some coverage and cost-sharing restrictions. CMS has told plans that they may waive or decrease cost-sharing for telehealth services in response to the coronavirus pandemic, as long as they do so equitably for all similarly situated participants. During the public health emergency, several Medicare Advantage plans eliminated or reduced cost-sharing for part or all telehealth services for subscribers.
Who Has Used Telehealth Services During the COVID-19 Public Health Emergency?

Awareness of Telehealth Availability
As of Fall 2020, nearly two-thirds of community-dwelling Medicare beneficiaries who say they have a usual source of care (64 percent, or 33.6 million beneficiaries), such as a doctor or health professional, or a clinic, reported that their usual provider offers telehealth appointments, up from roughly one-fifth (18 percent, or 6.1 million) beneficiaries who said their usual provider offered telehealth appointments six months after traditional Medicare expanded telehealth benefits for the COVID-19 pandemic (Figure 2; Table 1). (Around 95 percent of community-dwelling Medicare participants, or 52.7 million people, say they have a regular source of care.)
In contrast, just 13% of beneficiaries with a regular source of care indicated their physician does not now offer telehealth, a significant drop from the 52% who claimed their provider did not offer telemedicine prior to the COVID-19 epidemic.
Despite the fact that telemedicine availability has expanded throughout the pandemic, over a quarter of Medicare members with a primary care provider (23 percent or 11.9 million beneficiaries) do not know if their primary care physician now provides telehealth visits.
Across most demographic categories, the reported rates of beneficiaries who indicate their provider now offers telehealth were similar (Figure 3). However, a lower percentage of Medicare beneficiaries in rural areas than in urban areas said their provider currently offers telehealth (52 percent vs. 67 percent, respectively), and a higher percentage of rural beneficiaries say they don’t know if their usual provider offers telehealth appointments (30 percent vs 21 percent, respectively).
A higher percentage of Black Medicare beneficiaries with a primary care provider (23%) said their primary care provider does not now provide telehealth visits than White (12%) or Hispanic (15%) beneficiaries with a primary care provider. Furthermore, a higher percentage of Medicare beneficiaries who are both Medicare and Medicaid beneficiaries (19%) report their typical provider does not now provide telehealth visits than Medicare beneficiaries who are not both Medicare and Medicaid beneficiaries (12 percent ).
Use of Telehealth
Nearly half (45 percent, or 14.9 million beneficiaries) of Medicare members with a usual source of care who stated in the Fall of 2020 that their usual provider offers telemedicine during the pandemic (33.6 million beneficiaries) reported having a telehealth visit since July 2020. Medicare beneficiaries under 65 with long-term disabilities, Black and Hispanic beneficiaries, Medicare beneficiaries enrolled in both Medicare and Medicaid, and beneficiaries with multiple chronic conditions were more likely than others to report having a telehealth visit with a doctor or other health professional since July 2020. (Figure 4; Table 2).
Among Medicare beneficiaries who have a usual source of care and whose usual provider offers telehealth:
- More than half (53%) of beneficiaries under 65 (who qualify for Medicare due to a long-term disability) had a telehealth visit, compared to 42% of those 65 to 74 and 43% of those 75 and older.
- A higher percentage of Black (52%) and Hispanic (52%) Medicare beneficiaries report they had had a telemedicine visit than White (43%) beneficiaries.
- More than half of Medicare and Medicaid members (55%) had a telehealth visit, compared to 43% of Medicare beneficiaries who were not enrolled in Medicaid.
- Beneficiaries with six or more chronic conditions were more likely than those with zero or one chronic condition to have a telehealth visit (56 percent vs. 33 percent), and a half or more of Medicare beneficiaries with specific chronic conditions, such as diabetes (50 percent), a heart condition (50 percent), emphysema, asthma, or COPD (54 percent), depression (55 percent), and those who are immunocompromised, had a telehealth visit (59 percent ).
- Since July 2020, a similar amount of Medicare Advantage participants (45 percent) and normal Medicare enrollees (44 percent) had had a telehealth visit (Table 2).
- Based on the total population of community-dwelling beneficiaries, which also includes beneficiaries who said they did not have a telehealth visit, beneficiaries who do not know if their provider offers telehealth, and those without a usual source of care who were not asked about it, Medicare beneficiaries who report having a telehealth visit between the summer and fall of 2020 account for one out of every four Medicare beneficiaries overall (27 percent, or 14.9 million beneficiaries) (Figure 4, Table 2).
Notably, we observed no significant difference between the percentage of rural and urban Medicare beneficiaries who had a telemedicine visit among those with a regular source of care and whose regular provider offers telehealth (43 percent and 45 percent, respectively). Rural Medicare beneficiaries, on the other hand, were less likely than urban Medicare beneficiaries to have a telehealth encounter with a doctor or other health professional depending on the entire population in these categories (21 percent vs. 28 percent, respectively). This disparity is likely due to the fact that rural Medicare beneficiaries are more likely than urban Medicare beneficiaries to report they are unaware if their typical provider provides telehealth services (30 percent vs. 21 percent, respectively).
Similarly, we discovered that among Medicare beneficiaries with a regular source of care and a regular provider who offers telemedicine, a higher proportion of Black and Hispanic beneficiaries had a telehealth visit than White beneficiaries (52 percent , 52 percent , and 43 percent ). However, the difference in the percentage of Black and White Medicare beneficiaries who reported having a telemedicine visit was not statistically significant (30 percent vs. 26 percent), whereas a higher percentage of Hispanic beneficiaries had a telehealth visit than White beneficiaries (33 percent vs. 26 percent ). This is likely due to the fact that nearly a quarter of Black Medicare beneficiaries (23%) claim their typical provider does not provide telemedicine visits, compared to just 12% of White beneficiaries and 15% of Hispanic beneficiaries.
Find Medicare Plans in 3 Easy Steps
We can help find the right Medicare plans for you today
How Did Beneficiaries Access Telehealth Services?
The majority of Medicare beneficiaries with a typical source of care whose provider provides telehealth appointments utilized the service via phone (56 percent), compared to 28 percent who used video and 16 percent who used both telephone and video (Figure 5; Table 3). This might be due to the fact that, while more than 8 out of 10 Medicare recipients claim to have internet access (83 percent), a lesser percentage (64 percent) claim to own a computer or a smartphone (70 percent) (Figure 6, Table 4).
There are noticeable discrepancies in how beneficiaries have received telehealth services throughout the pandemic and the availability of technology that permits access to telehealth, for example, based on demographic characteristics:
- Two-thirds (65%) of Medicare beneficiaries aged 75 and older had a telephone-only telehealth visit, compared to just over half (52%) of those aged 65 to 74, findings that likely reflect the smaller share of Medicare beneficiaries aged 75 and older who report having internet access (74 percent vs. 89 percent) or owning a computer (56 percent vs. 74 percent) or smartphone (56 percent vs. 74 percent) (53 percent vs. 80 percent ).
- Six in ten Hispanic Medicare beneficiaries (61%) had a phone-only telehealth visit, compared to 54 percent of White beneficiaries. This is likely due to the fact that a smaller share of Hispanic Medicare beneficiaries than White beneficiaries report having internet access (67 percent vs. 86 percent), and a much smaller share of Hispanic beneficiaries say they own a computer (34 percent vs. 71 percent ). Similarly, just 42% of Black Medicare beneficiaries own a computer, compared to 71% of White beneficiaries, yet there was no significant difference in the percentage of beneficiaries reporting a telephone-only telehealth visit between Black and White beneficiaries.
- Rural beneficiaries were more likely than urban beneficiaries to report having a telephone-only telehealth visit (65 percent vs. 54 percent), which is likely due to rural beneficiaries’ lower rates of internet access (78 percent vs. 84 percent) and ownership of computers (58 percent vs. 66 percent) or smartphones (58 percent vs. 66 percent) (60 percent vs. 72 percent ).
Looking to the Future: Expanding Medicare Coverage of Telehealth Beyond the Pandemic

According to our research, one out of every four Medicare beneficiaries had a telehealth visit during the COVID-19 public health emergency, indicating a significant rise in utilization since before the pandemic. Our discovery that a higher percentage of beneficiaries with disabilities, low incomes, and living in communities of color have used telehealth suggests that the temporary expansion of telehealth coverage may be assisting some of Medicare’s most vulnerable populations in maintaining access to needed care.
Efforts to raise awareness of covered telehealth services under Medicare during the public health emergency could help to broaden its reach, given our finding that a quarter of Medicare beneficiaries overall (and an even higher share of those in rural areas) do not know if their doctor currently offers telehealth.
Many legislators have indicated support for expanding some or all of the existing flexibilities around telehealth services under Medicare beyond the public health emergency. Proposals to permanently cover some of the telehealth expansions provided during the public health emergency, expand Medicare-covered mental health services and evaluation and management services administered via telehealth, and expand the scope of providers eligible for payment for telehealth services covered by Medicare are among the telehealth-related bills introduced in the 117th Congress. Other proposals attempt to analyze the impact of increased telehealth services on patient care quality and program cost.
A telehealth visit must be done with two-way audio/video technology under Medicare’s current telehealth benefit, although a limited number of telehealth services can be delivered to patients through audio-only telephone under the current public health emergency waiver. Given that the majority of Medicare beneficiaries in our study said they only used telephones to access telehealth services, an expanded telehealth benefit that requires two-way video communication could be a barrier to care for subgroups of the Medicare population who used telephones more than video-capable devices during the pandemic.
After the public health emergency expires, MedPAC recommends that Medicare continue a modified form of extended telehealth coverage for another year or two, providing Medicare time to analyze the impact of telehealth use on overall costs, access, and quality of treatment. During this additional time, MedPAC recommends that Medicare pays for certain telehealth services regardless of where a beneficiary lives; cover some additional telehealth services beyond those covered prior to the public health emergency if clinical benefit is possible, and cover audio-only telehealth visits if clinical benefit is possible.
After the public health emergency, MedPAC recommends that reimbursement for telehealth services revert to the lower facility-based payment rate in force before the pandemic and that providers should not be able to waive or decrease beneficiary cost-sharing.
Telehealth coverage beyond the public health emergency might have an impact on patient treatment quality, as well as program and beneficiary costs. Expanding telehealth coverage has the potential to enhance access to essential treatment, but it’s unclear whether it’ll result in a rise or fall in the total program cost. Some telehealth services, such as behavioral health care visits, maybe alternatives for in-person care, while increased availability of telehealth may result in an overall rise in visits and expenses.
Other telehealth services may not be able to completely replace the need for (or occurrence of) an in-person visit, such as a visit to examine a skin rash or a visit if lab work is required. The Administration could potentially gain insights based on telehealth use by enrollees in Medicare Advantage plans, or by testing different approaches through the Center for Medicare and Medicaid Innovation models, in order to build evidence on the cost and quality impacts of telehealth use in Medicare.
Concerns regarding the possibility of fraudulent conduct accompany the prospective growth of telehealth coverage. In recent years, there have been numerous substantial fraud instances involving telehealth firms, most of which included the submission of false claims to Medicare and other insurers for things, services, and tests that were never supplied or administered to patients.
The Office of Inspector General (OIG) of the Department of Health and Human Services is conducting several studies to determine the appropriateness of telehealth use during the public health emergency, including an analysis of provider billing patterns to identify providers who could jeopardize program integrity and an audit of telehealth services under Part B to ensure that services meet Medicare requirements. Outlier physicians who provide more telehealth services than others should be scrutinized more closely by Medicare, and in-person visits should be required before clinicians may prescribe high-cost equipment or services for patients, according to MedPAC.
During the coronavirus epidemic, many people with Medicare were able to get medical treatment because of a brief increase in telehealth coverage. Given that the public health emergency’s temporary waiver of restrictions on telehealth coverage under Medicare will expire with the end of the emergency, the question of whether and how to ensure continued access to these services while balancing concerns about the quality of care and spending looms large.
Data and Methods: This research utilizes survey data from the Centers for Medicare & Medicaid Services (CMS) Medicare Current Beneficiary Survey (MCBS) Fall 2020 COVID-19 Community Supplement for community-dwelling Medicare enrollees. From July 2020 through Fall 2020, the MCBS Fall COVID-19 supplement contains additional survey items aimed to measure Medicare beneficiary’s access to care and use of telehealth services.
Beneficiaries who responded yes to the question “Is there a specific doctor or another health professional, or a clinic you normally attend when you are unwell or for advice about your health?” were used to calculate the proportion of Medicare beneficiaries whose provider offers telehealth. “Does your typical provider provide telephone or video appointments, so you don’t have to physically visit their office or facility?” was asked of 9,216 out of 9,686 responses. There were 5,644 positive responses.
“Since July 1, 2020, have you had an appointment with a doctor or other health professional by telephone or video?” beneficiaries with a usual source of care whose usual provider offers telehealth appointments were asked in order to determine the share of Medicare beneficiaries who had a telehealth visit. (2,515 people responded affirmatively). “Did your normal provider provide telephone or video appointments before the coronavirus pandemic?” was also questioned of beneficiaries with a regular source of care whose provider offers telehealth. (1,035 people responded affirmatively).
Beneficiaries who had a telehealth visit since July 2020 were asked, “Was it a telephone appointment, video appointment, or both?” to identify how they accessed telehealth appointments. The majority of Medicare members who had a telehealth visit since July 2020 (n=1,460) did so over the phone, while fewer (n=653) or both (n=393) did it over the phone and video.
Beneficiaries were only questioned about their usage of telehealth if they indicated affirmatively that they had a regular source of treatment and that their regular provider provided telemedicine, based on the questionnaire skip patterns. We constructed a categorical variable that includes beneficiaries whose provider did not provide telehealth or it was unknown in order to assess the percentage of Medicare beneficiaries who had a telehealth visit among all Medicare beneficiaries. The variable was divided into three groups: 1) the usual provider offers telemedicine and the beneficiary has had a telehealth visit (n=2,515); 2) the typical provider offers telehealth but the beneficiary has not had a telehealth visit (n=3,074); 3) the usual provider does not offer telehealth or it is unclear (n=4,097).
All statistical tests yielded significant results, with p0.05 deemed statistically significant.